Home birth
This page is about having a home birth with King’s. It covers the benefits and the risks of a home birth, how to plan for a home birth, and what you can expect from the midwives providing your care.
What is a home birth?
At a home birth, midwives attend your home to provide care during labour and in the hours after the birth.
Each birth is attended by two midwives. Usually, one midwife arrives to provide labour care and the second midwife attends closer to the time of birth.
There may be a changeover of midwives during your home birth, depending on how long they are with you.
What are potential benefits of a home birth?
Benefits include:
- the birth is more likely to be attended by a midwife you know
- a lower likelihood of an intervention such as an instrumental birth (forceps or ventouse) or an episiotomy (a cut in the area between the vagina and anus)
- some research has found those giving birth at home tend to use less pain relief
- reduced risk of perineal tear
- some research has found those who have a home birth feel more in control during their labour
Other potential benefits are:
- you don’t have to travel to hospital
- you will be in a familiar place and may feel more comfortable in your own home
- you can have as many birth partners as you like
- you can recover in the comfort of your home
- if you already have children, it may reduce the need for childcare cover during labour and immediately after the birth
- you are more likely to see the same midwife throughout your pregnancy care
What are potential risks and considerations of a home birth?
- During or after the birth you may need, or choose, to transfer to hospital. Some research shows that around 45% of women having their first baby transfer to hospital during or just after birth. For second or subsequent births, this is around 12%.
- For low-risk first-time births, the chance of a problem with your baby’s health straight after home birth is 9.3 in 1,000, compared to 5.3 in 1,000 in doctor-led units. In second and subsequent births, there is no difference in this risk when home births and doctor-led unit births are compared.
- It is unusual to be transferred to hospital as an emergency. But if you are, it will take longer to get emergency care than if your labour started in hospital.
- Very rarely the home birth service may be suspended at short notice if the maternity service is very busy.
- There are fewer pain relief options at home. You can only have pethidine or an epidural in hospital.
Who can have a home birth?
By law you have the right to choose where to give birth.
Giving birth at home is a safe option if you have had an uncomplicated pregnancy and, in particular, if you have previously had a straightforward vaginal birth and you do not have any medical complexities.
If you have certain medical or pregnancy conditions, we may advise that hospital is the safest place to have your baby.
However, providing the care you want is important. If you would like a home birth and have an existing medical condition, speak to your midwifery team or contact one of the midwifery teams that provide a home birth service (Birchtree and Phoenix). We will look at your individual circumstances to help you decide the best place to give birth.
For more information about your rights around birth, visit the Birthrights website
Who attends home births?
There are two midwife teams that provide a home birth service – Birchtree and Phoenix. They are experienced in supporting birth at home, and can also recognise when it may be necessary to transfer care to the labour ward for extra support.
If you choose a home birth, you will be cared for by one of these teams. They will support you during your pregnancy and birth, and in the postnatal period.
You will have a named midwife, who will see you for most of your planned midwifery appointments. Most of these will be at your home, but you may also need to come into clinic at some points in your pregnancy. Scans and doctor-led appointments will be at the hospital.
We cannot guarantee that your named midwife will attend your birth, as our midwives do not work 7 days a week. Instead, each team works together to provide a 24/7 on-call service for births. Please expect to meet and become familiar with the rest of your midwifery team during your pregnancy.
When and how should I contact the midwives to attend the birth?
Your midwifery team will give you phone numbers for all team members. We provide cover every day to assist you over the phone.
- If you are less than 36 weeks pregnant and think you may be in labour, call the 24/7 Maternity Telephone Assessment Line.
- If you are 36 weeks pregnant or more, call your named midwife. If needed you can also phone other members of the midwifery team. If you are phoning out of hours (weekends, bank holidays, and 5pm to 8am Monday to Friday) call your team’s on-call midwife. We will give you an on-call list when you reach 36 weeks of pregnancy, so you know who to contact out of hours.
When you call, we will ask you some questions to help decide if it is time for the midwife to attend you.
If this is your first baby, we suggest you call when you are having 3 to 4 contractions every 10 minutes, lasting for 1 minute, for the past hour.
If you are having a second or subsequent baby, call as soon as your contractions are strong and regular, as these births can be quicker.
If your waters break (with or without contractions) call us straight away. It is important to let us know immediately if your waters appear green, brown, or yellow.
It may take up to an hour for the midwife to arrive at your home. Once they have arrived they will offer to assess you to see if you are in established labour. If you are not yet in established labour, the midwife may leave and come back later.
How will the midwife monitor me and my baby during labour?
Throughout your labour the midwife will offer to take your observations, including your blood pressure, heart rate, temperature, oxygen levels, and breathing rate. They will also observe the strength, length, and frequency of your contractions. If your waters have broken they will offer to check their colour, to ensure they are clear.
You will be encouraged to empty your bladder often and offered a urine test (urinalysis) to make sure you do not have harmful levels of protein, ketones, or infection cells in your urine.
Your midwife will encourage you to drink regularly to stay hydrated, and to eat light snacks to maintain your energy levels.
They will offer to listen to your baby’s heartbeat every 15 minutes in the first stage of labour (before your cervix is fully dilated) and every 5 minutes in the second stage (when your cervix is fully dilated and you want to push). They will also ask to listen immediately after each contraction for 60 seconds, to ensure the baby’s heart rate remains normal.
They will use a handheld listening device to listen to your baby’s heartbeat.
What equipment do midwives bring?
Midwives bring the equipment needed to provide safe labour care in your home. This includes, but is not limited to:
- equipment to monitor your blood pressure, heart rate, temperature, oxygen levels, and breathing
- a device to listen to baby’s heartbeat
- a mirror
- a torch
- gas and air
- an injection of oxytocin. If you choose to, this can be injected into your thigh shortly after the birth, to help deliver your placenta (afterbirth)
- equipment to stitch minor tears, including local anaesthetic
- weighing scales
- vitamin K for baby (injection or oral drops)
- pain relief for after the birth
Midwives also bring equipment to manage emergencies before further help arrives, including:
- neonatal resuscitation and suction equipment
- adult resuscitation equipment
- medication to manage bleeding after the birth
- cannulas for intravenous (IV) fluids
- blood-taking equipment
- catheterisation tubes and bags, if needed to empty your bladder
We do not carry continuous fetal monitoring equipment, scanning equipment, antibiotics, blood pressure medication, forceps, or a ventouse. If these are needed we will advise transferring to hospital.
What pain relief options are available at home?
Ways of managing pain at home include:
- massage
- a hot water bottle
- a TENS (transcutaneous electrical nerve stimulation) machine. You can hire or buy these. We recommend using a pregnancy-specific one, which will have a boost button you can use during contractions.
- having a shower
- a birth pool. You can buy or hire these, ideally at around 36 weeks of pregnancy. Your birthing partner will be responsible for filling the pool, maintaining water temperature, and emptying the pool. It should come with liner, hoses, hose attachments, and a pump to empty the pool. Plastic sheets and towels can be useful to protect the floor. It is important your midwives can access all sides of the pool, and there is space outside the pool to give birth, in case you decide to get out of the water.
- paracetamol (can be bought over the counter)
- gas and air (entonox). The midwife will bring this.
- sterile water injections – these are when small amounts of sterile water are injected into the skin around your lower back to relieve back pain. The midwife will bring these.
Stronger pain relief, such as pethidine or an epidural, is not available at home births. If you decide during labour that you would like stronger pain relief, we will arrange for you to be transferred to hospital for this.
How many birthing partners can I have at home?
You can have as many birthing partners as you like at home. For some people, this might be just their partner. Others might feel more comfortable with more people around them.
Your children are welcome to be part of the birth if this is the right decision for your family. However, it is important there is another adult present to care for them, in case you are transferred to hospital for any reason.
You may choose to hire a doula for your labour. Doulas are non-medical professionals that support you physically and emotionally during birth. We welcome doulas as part of your birthing team but believe it is important to meet with them before labour, so we work well as a team on the day.
What do I need to supply for a home birth?
Only the essential items listed below are necessary. You may also wish to supply some of the optional items to help feel more comfortable.
Essential items:
- towels – five adult size and five hand towel size
- baby provisions – clothes, hats, wipes or cotton wool balls, and nappies
- food and drinks for you and your partner (we recommend non-fizzy electrolyte drinks, such as sports drinks).
- maternity pads or super-absorbent period pads, for normal postpartum bleeding
- mobile phone signal
Optional items:
- a birthing pool – if you would like to hire one, please talk to your midwife
- plastic coverings to protect furniture
- disposable changing mats or incontinence pads – useful to protect furniture when your waters have broken, and during normal postpartum bleeding
- a birthing ball
- affirmation cards
- music or a hypnotherapy track played through a speaker or headphones (we recommend making two playlists – one for relaxation and one for boosting energy)
- eye mask or ear plugs if you need to focus
- battery-powered candles or fairy lights, to create a calm atmosphere
- massage oil
- aromatherapy oils
- a cup or bottle with a straw, so you won’t need to tip back your head to drink, which can be distracting in labour
It is also useful to pack a birth bag to have in or near your birth space, which include pads, nappies, clothes for you and baby, a wash bag, and any other items you want. This is useful so that the midwives can easily locate your essentials during and after labour, but also important if you need to transfer into the hospital.
What happens after a home birth?
After birth, if you and baby are well and there are no complications, there will be no need to transfer you to hospital. Our midwives will support you with:
- skin-to-skin contact (holding your bare baby on your bare tummy or chest)
- delayed cord clamping (otherwise known as ‘wait for white’)
- delivering your placenta
- feeding your baby.
They will offer to check your perineum for any tears and will be able to repair most tears at home under local anaesthetic.
They will help maintain a peaceful and undisturbed environment, particularly for your golden hour – the very first hour of your baby’s life. This is when you and your baby can start getting to know each other, and have lots of skin-to-skin contact. Weighing and examining your baby can wait until you are ready.
Our midwives will then stay for a few hours to ensure you and your baby are well, and to complete the necessary paperwork. They will then return around 6 to 18 hours after birth to check on you, depending on the time you give birth.
Our midwives are trained in the Newborn and Infant Physical Examination (NIPE). This is a thorough examination of your baby, concentrating on screening for problems with their eyes, heart, hips, and testes (if applicable). The NIPE is recommended in the first 72 hours of life.
Our midwives will usually come and see you at home on days 1, 3, 5 and 10 after the birth. It is then up to you how much support you would like from them.
What if there are problems during the birth?
If your midwife is concerned about you or your baby, you will be advised to transfer to the hospital. This may be during or after labour.
There are many reasons to transfer to hospital, and many are not an emergency.
Reasons include:
- concerns about your baby’s heartbeat
- abnormal observations, such as raised blood pressure, heart rate, or temperature
- your baby has passed meconium (their first poo) into your waters (amniotic fluid)
- your labour is progressing slower than is usual
- abnormal bleeding
- the placenta (afterbirth) is slow to deliver
- significant tearing to your vulva or perineum that needs repairing by a doctor in hospital
- your baby needs assistance to breath at birth
- your baby’s shoulders were slow to be delivered
- concerns with your baby’s breathing or temperature after the birth
- you wish to transfer for any reason, such as stronger pain relief
An ambulance would take you to hospital. A midwife and one birthing partner also go in the ambulance.
We have a direct line to the London Ambulance Service (LAS). All home birth midwives have had training with LAS paramedics to ensure safe and efficient multi-disciplinary teamwork.
In an emergency, LAS should provide a response time of 8 to 15 minutes. If your transfer is not an emergency (there is no threat to your or your baby’s life) the response time may be longer.
The average transfer time in emergencies, from phoning for an ambulance to arriving on Nightingale Birth Centre at King’s, is around 30 to 40 minutes.
If you have a home birth, it will take longer to access hospital emergency services compared to if your labour started at the hospital. Because of this, home birth midwives and paramedics are trained to manage emergencies during transfer to hospital. This means that emergencies can be managed until arriving with the emergency team at the hospital.
What are the alternatives to a home birth?
Other options at King’s are our midwife-led birthing rooms, or the doctor-led labour ward. For more information go to our page about Where can I choose to give birth?
What if I change my mind during my pregnancy or I am advised to give birth in hospital?
If you change your mind about having a home birth or we advise you have a hospital birth, your existing midwife team will continue to provide your antenatal and postnatal care.
When you go into labour, a member of your midwife team will try to attend your labour at the hospital. If they are not able to do this due to high demand on the home birth service, our hospital colleagues will support you and your baby during your labour.
What happens if no midwives can attend my home birth?
In very rare circumstances, when there are multiple ongoing home births, or demand for maternity services is very high, we may be unable to attend you at home. In the unlikely event this happens when you go into labour, we will recommend you come into the hospital and give birth in the midwifery-led unit on Nightingale Birth Centre.
We recognise that this may be disappointing. This only happens on very rare occasions, when is it needed to ensure safe care.
Contact us
Please complete the Antenatal self-referral form and tick that you are interested in a home birth. We will then contact you about your first appointment, known as your booking appointment.
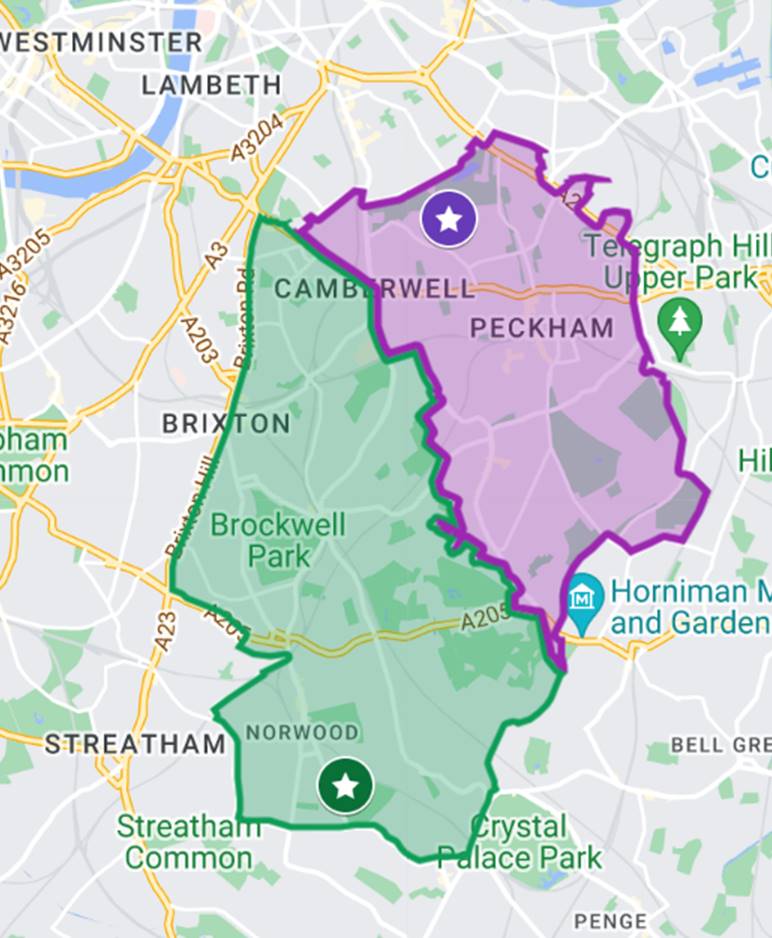
If you are already booked in for antenatal care at King’s and are now interested in having a home birth, please email the Birchtree or Phoenix team with your name, hospital number (if you have one), and postcode. The picture map at the end of this section shows the area each team covers:
Birchtree team
Catchment area in green on picture map.
- Catchment area includes, but not limited to: SE5, SE24, SE27, SE21, SW9 – Loughborough Junction, Brixton, Herne Hill, Tulse Hill, Norwood, West Norwood, West Dulwich, North Dulwich, and Camberwell
- Email: [email protected]
Phoenix team
Catchment area in purple on picture map.
- Catchment includes, but not limited to: SE5, SE15, SE22 – East Dulwich, Peckham, Newlands, Nunhead, and Camberwell.
- Email: [email protected]